“`html
Effective Ways to Modify Your Gastroparesis Diet for Better Symptoms in 2025
Living with gastroparesis can be challenging, particularly when it comes to managing your diet. In 2025, it’s crucial to adopt a gastroparesis diet that caters to your nutritional needs while minimizing symptoms. This article provides effective strategies for modifying your diet, allowing you to better manage your symptoms.
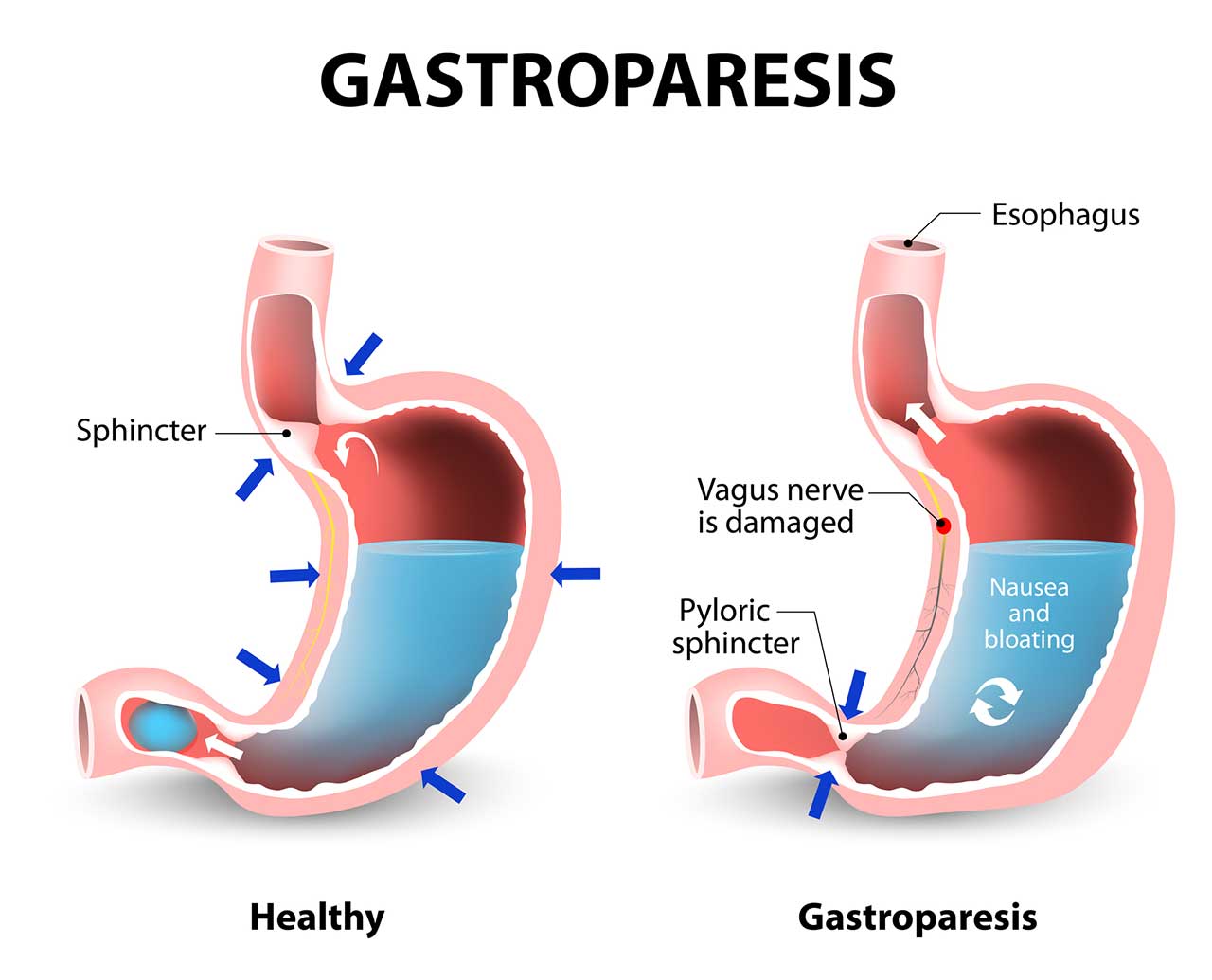
Understanding Gastroparesis and Its Dietary Needs
Gastroparesis is a condition that affects the normal spontaneous movement of the muscles in the stomach. This can lead to delayed gastric emptying, resulting in various challenging symptoms. Following an effective gastroparesis meal plan is essential for symptom management and overall well-being. A tailored diet can ensure that you get the nutrients you need while avoiding foods that exacerbate your condition. This often involves a combination of low-fiber and low-fat dietary options to help ease digestion.
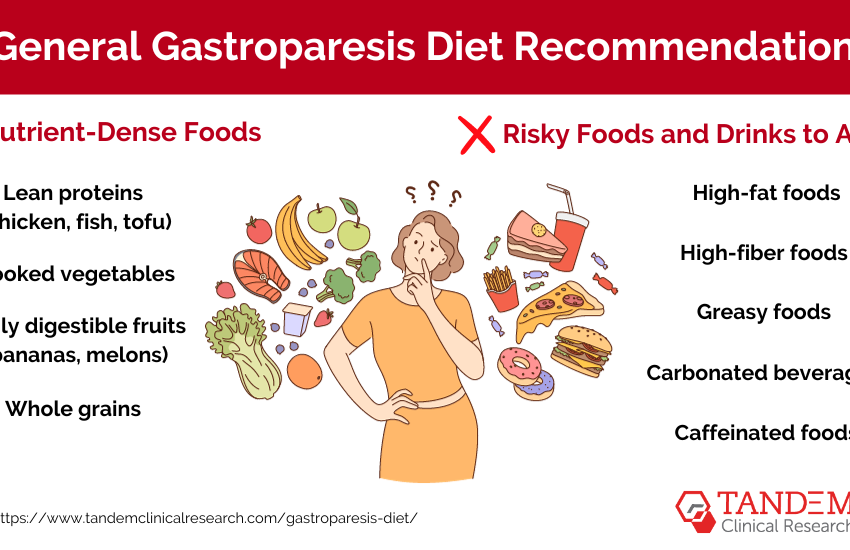
Low-Fiber and Low-Fat Diet Principles
A low-fiber diet is crucial for individuals with gastroparesis because fiber can slow gastric emptying. Opting for a low-fat diet can also reduce the workload on your stomach. Incorporate foods such as white rice, plain pasta, and skinless chicken into your meals. These options are generally easier to digest and less likely to cause discomfort. Remember, the key is to make these dietary adjustments while ensuring you still maintain a good balance of nutrients.
Importance of Small Frequent Meals
Consuming small frequent meals rather than large portions can help manage symptoms effectively. When the stomach is less full, it can empty more easily, improving comfort and easing nausea. Aim for five to six small meals per day, including easy-to-digest options such as mashed potatoes or soft-cooked carrots. This approach not only helps maintain energy levels but also tailors your individualized diet to your personal tolerances and preferences.
Choose Soft and Liquid Foods
Soft foods and liquid meals are often recommended due to their easy digestibility. Foods like yogurt, custards, smoothies, and soups can be comforting while providing necessary nutrients. Additionally, you may want to consider a diet enriched with high-calorie snacks like protein shakes, which can offer energy-boosting benefits without overwhelming your digestion.
Navigating Nutritional Supplements and Food Modifications
Incorporating nutritional supplements into your gastroparesis diet can help fill any gaps left by your adjusted meals. Consult with a healthcare provider about the best nutritional supplements for your specific condition. These can play a key role in maintaining hydration importance and supporting your overall health when traditional food intake is compromised.
Protein and Nutrient-Dense Foods
Consider focusing on high-protein foods such as eggs, fish, and legumes, which can promote muscle strength and overall health. Pairing these with nutrient-dense foods, like mashed sweet potatoes or smoothies made from fruit, can help ensure balanced micronutrient intake. These modifications are essential as they provide the necessary building blocks without taxing the digestive system too much.
Cooking Techniques and Food Texture Modification
Utilizing specific cooking techniques can also make a significant difference in how well food is tolerated. Cooking methods such as steaming or boiling can soften food, making it easier to digest and more palatable. Moreover, modifying food texture, such as pureeing certain items, can lead to more comfortable eating experiences.
Identifying Trigger Foods and Managing Symptoms
One effective strategy for managing your symptoms is identifying and avoiding trigger foods that worsen discomfort. Keeping a food diary can assist in tracking what you eat and how it affects your symptoms. This awareness facilitates better food choices, helping you to avoid fibrous vegetables and other problematic items.
Meal Timing and Portion Control
Practicing mindful eating by paying attention to meal timing and portion control can have a profound impact on your symptom management. Eating smaller portions allows for better digestion, and spacing meals adequately prevents overloading the stomach and can mitigate the nausea often associated with gastroparesis.
Consulting a Dietitian and Making Dietary Adjustments
Consulting a dietitian who specializes in gastrointestinal motility disorders is highly beneficial. They can provide personalized recommendations and assist you in adjusting your dietary habits based on your symptoms, preferences, and lifestyle. You can collaborate to create an individualized nutrition plan tailored to your unique needs.
Key Takeaways for Managing Gastroparesis Through Diet
Implementing effective dietary strategies is crucial for managing gastroparesis. Here are key takeaways:
- Focus on a low-fiber, low-fat diet for symptom relief.
- Prioritize small frequent meals to ease digestion.
- Incorporate soft and liquid foods to avoid discomfort.
- Identify trigger foods and make dietary adjustments accordingly.
- Consult a dietitian for expert guidance on your individualized diet.
Customizing your gastroparesis diet can significantly enhance your quality of life by improving symptom management. By following the strategies outlined above, you can regain control over your digestive health.
FAQ
1. What are some effective liquid meals for gastroparesis?
Effective liquid meals for gastroparesis include smoothies, broth-based soups, and protein shakes. These options are easy to digest, can provide essential nutrients, and are less likely to trigger symptoms.
2. How can I balance my nutrient-dense foods while avoiding triggers?
Balancing your nutrient-dense foods while avoiding triggers involves careful planning. Focus on foods that provide high energy and nutrients without common trigger ingredients. For example, opt for mashed bananas instead of heavier fibrous fruits.
3. Why is meal timing important in a gastroparesis diet?
Meal timing is crucial as it allows the stomach enough time to process food. Spacing out small meals enhances digestion and reduces feelings of fullness, which can help manage symptoms.
4. What role does hydration importance play in managing gastroparesis?
Staying well-hydrated is vital since many individuals with gastroparesis struggle with fluid intake. Sufficient hydration supports digestive health and can prevent constipation, alleviating some gastro symptoms.
5. How can I modify recipes to make them suitable for a gastroparesis diet?
To modify recipes, consider cooking foods thoroughly to soften them, using pureed techniques, or reducing fibrous ingredients. These adjustments can help ensure better tolerance and ease of digestion.
Keeping awareness of your specific dietary needs and making informed choices will allow you to navigate the challenges of gastroparesis effectively.
“`